4 WAYS TO DECREASE YOUR PLANTAR FASCIA HEEL PAIN
1 out of 10 people experience Plantar Heel Pain (more commonly known as Plantar Fasciitis or Plantar Fasciopathy). 8% of running injuries are caused by Plantar Heel Pain (1,2).
Those with Plantar Heel Pain typically experience:
- Pain that is worse in the morning (with the first few steps out of bed felt noticeably) or pain after prolonged sitting (3).
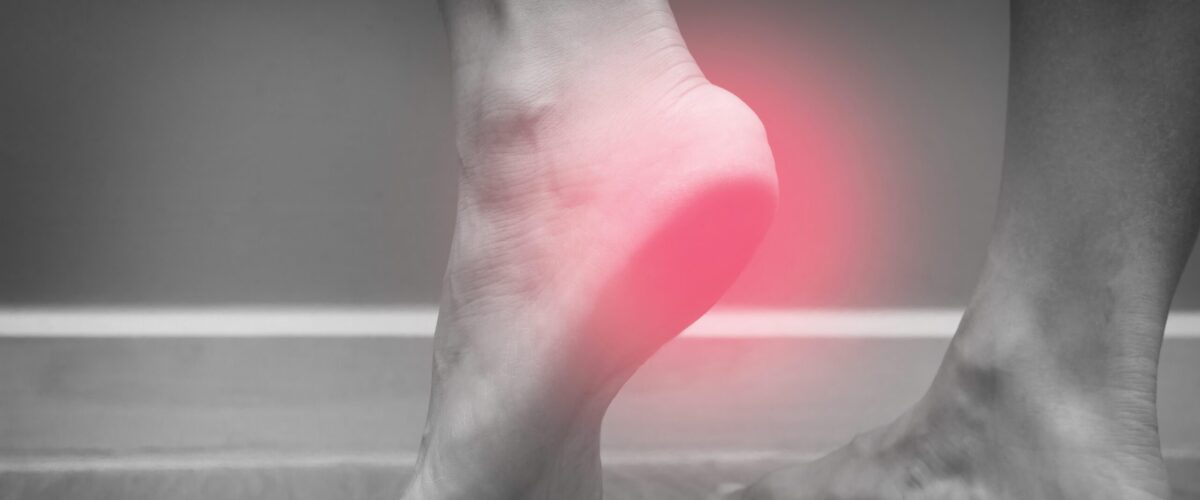
- A sharp pain localised under the heel (see Image #1)
- Pain can decrease during the day however it often worsens in the evening (3).

2 common presentations of people who experience Plantar Heel Pain (but not limited to!);
- The athlete with a large training volume
- Often an increase in kilometres run or increase in number of running sessions per week.
- The inactive and overweight middle-aged person
- Often work in a job that involves standing for long periods
Other important notes:
- Imaging scans (such as ultrasound or MRI) can aid the clinician’s assessment but is not required to make a diagnosis (3)
- Only two thirds of people with plantar heel pain have heel spurs on x-ray scans (see image #2). Half of those with heel spurs do not have pain. This suggests that heel spurs are an x-ray finding but not a diagnosis (4).
- If heel pain has been felt for 7 months or longer, and the person is of female gender, 40 years of age or less and bilateral heel pain (pain felt both right and left heels) this can lead to a worse prognosis.

4 SIMPLE WAYS TO DECREASE YOUR PLANTAR FASCIA HEEL PAIN:
1. ACTIVITY MODIFICATION
- For those experiencing significant pain during or after running it may mean changing your activity to cycling on a bike or swimming for a period. Then consider gradual increases in your running provided pain is on the low side – it is recommended that you discuss this with a physiotherapist who can help work at a safe running plan with you.
- For those who work in jobs that involve standing for long periods; consider (where possible) to have some periods sitting down. You may also consider other activities outsides of work that involve standing or being “on your feet”; such as walking the dog after work, spending several hours cooking or even standing on the sidelines watching the children’s recreational sport – decreasing this time on your feet can help towards decreasing your heel pain.
2. STRENGTHENING!
- A study comparing a 3 month period of stretching of the plantar fascia compared to strengthening showed that strengthening had greater benefit following 3 months of performing the exercise protocol (5).
- This strengthening exercise involves the big toe/s positioned on a rolled up towel aiming for the big toe/s to point as far upwards as possible (see video below) – this places greater strain to the plantar fascia. Perform this over the edge of a step.
- Raise up in 3 seconds, hold for 2 seconds and slowly lower in 3 seconds on the way down.
- Aim for 2-3 sets of 8-12 repetitions and gradually progress through the different variations. Aim to perform these every second day.
- Performing this exercise with some pain is generally safe to do. However if pain is becoming sharp or significantly worsening then consider stopping this. It’s important to mention that before considering doing this exercise; if you are experiencing heel pain that you are assessed by a physiotherapist.
3. WEIGHT MANAGEMENT
- A risk factor for the development of plantar fascia heel pain in a non-athletic population is being overweight (6).
- Only one study has looked at the effect of weight loss on decreasing plantar heel pain showing a significant benefit in reducing symptoms (7).
- If you think you may be overweight; an assessment from your GP or a dietician could determine if this could be contributing to your heel pain. Advice from a dietician can help decrease weight.
4. ORTHOTICS/SHOE INSOLES
- Research suggests that an insole with an arch may help reduce Plantar Fascia Heel Pain in the initial stage for up to a 6 week period (8). Beyond this period of time has been shown to have no further beneficial effect (8).
- This research has shown that “off the shelf” (pre-fabricated) orthotics (with a raised arch) were equally as effective as custom made orthotics to reduce Plantar Fascia Heel Pain and improve function (8). “Off the shelf” orthotics are an inexpensive option that may help reduce your heel pain.
- Another study found that contoured sandals provide a similar beneficial effect to an “off the shelf” shoe insert in reducing Plantar Fascia Heel Pain and both of these had a superior effect when compared to a flat thong (see image #3) (9).
- Taping of the foot, similar to an “off the shelf” orthotic, can have a short term effect in helping reducing plantar heel pain. The different taping techniques that have been researched all showed to help reduce Plantar Fascia Heel Pain (10,11,12). A physiotherapist can help with this.

If you are experiencing heel pain or lower leg/foot pain; book an appointment now at Continuum Physiotherapy for further guidance as to how to reduce your heel pain.
- Taunton, J. E., Ryan, M. B., Clement, D. B., McKenzie, D. C., & Lloyd-Smith, D. R. (2002). Plantar fasciitis: a retrospective analysis of 267 cases. Physical Therapy in Sport, 3(2), 57-65.
- Crawford, F., & Thomson, C. E. (2003). Interventions for treating plantar heel pain. Cochrane Database of Systematic Reviews, (3).
- Crawford, R. (2011). Diagnosis and treatment of plantar fasciitis. Am Fam Physician, 84(6), 676-82.
- McMillan, A. M., Landorf, K. B., Barrett, J. T., Menz, H. B., & Bird, A. R. (2009). Diagnostic imaging for chronic plantar heel pain: a systematic review and meta-analysis. Journal of Foot and Ankle Research, 2(1), 32.
- Rathleff, M. S., Mølgaard, C. M., Fredberg, U., Kaalund, S., Andersen, K. B., Jensen, T. T., … & Olesen, J. L. (2015). High‐load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12‐month follow‐up. Scandinavian journal of medicine & science in sports, 25(3), e292-e300.
- Van Leeuwen, K. D. B., Rogers, J., Winzenberg, T., & van Middelkoop, M. (2016). Higher body mass index is associated with plantar fasciopathy/‘plantar fasciitis’: systematic review and meta-analysis of various clinical and imaging risk factors. Br J Sports Med, 50(16), 972-981.
- Boules, M., Batayyah, E., Froylich, D., Zelisko, A., O’Rourke, C., Brethauer, S., … & Kroh, M. (2018). Effect of surgical weight loss on plantar fasciitis and healthcare utilization. Journal of the American Podiatric Medical Association.
- Whittaker, G. A., Munteanu, S. E., Menz, H. B., Tan, J. M., Rabusin, C. L., & Landorf, K. B. (2018). Foot orthoses for plantar heel pain: a systematic review and meta-analysis. Br J Sports Med, 52(5), 322-328.
- Vicenzino, B., McPoil, T. G., Stephenson, A., & Paul, S. K. (2015). Orthosis-shaped sandals are as efficacious as in-shoe orthoses and better than flat sandals for plantar heel pain: a randomized control trial. PLoS One, 10(12), e0142789.
- El Salam, M. S. A., & ELhafz, Y. N. A. (2011). Low-dye taping versus medial arch support in managing pain and pain-related disability in patients with plantar fasciitis. Foot & ankle specialist, 4(2), 86-91.
- Hyland, M. R., Webber-Gaffney, A., Cohen, L., & Lichtman, S. W. (2006). Randomized controlled trial of calcaneal taping, sham taping, and plantar fascia stretching for the short-term management of plantar heel pain. Journal of Orthopaedic & Sports Physical Therapy, 36(6), 364-371.
- Radford, J. A., Landorf, K. B., Buchbinder, R., & Cook, C. (2006). Effectiveness of low-Dye taping for the short-term treatment of plantar heel pain: a randomised trial. BMC musculoskeletal disorders, 7(1), 64.